Dive Brief:
- The leaders of the Senate HELP Committee on Thursday proposed a wide-ranging and ambitious package of healthcare bills, including measures addressing surprise medical billing, price transparency, interoperability, drug costs and public health.
- One bill put forward would require commercial insurers to make claims data and expected out-of-pocket costs available to patients through application programming interfaces (APIs) and ensure that patients have full access to their electronic health records — in line with two proposed rules HHS released earlier this year.
- Another provision bans gag clauses in contracts between providers and health plans that prevent the release of cost and quality information or de-identified claims data. It also would create a national all-payer claims database and designates a nonprofit, nongovernmental entity to study how to reduce healthcare costs.
Dive Insight:
Initial industry reaction to the proposals was relatively muted as groups said they were still reviewing the draft bills. The American Hospitals Association praised some of the public health provisions but said it was “concerned about several of the proposals that would allow the government to intrude into private commercial contracts between providers and insurers.”
AHA called out a ban on all-or-nothing clauses, which require health plans to contract with all providers in a system or none of them. The hospital group said they “could lead to even more narrow networks with fewer provider choices for patients, while adversely affecting access to care at rural and community hospitals.”
Analysts at Jefferies, however said a ban on anticompetitive contract elements should benefit for-profit hospital chains like Community Health Systems, Tenet and HCA “that offer high quality services as competitive prices.”
America’s Health Insurance Plans said it supports “many of the principles” outlined in the proposals and didn’t single out any provisions for attack. “We support transparency that allows consumers and patients to get information that is clear, helps them make informed decisions about their care, and leads to lower costs for them,” the payer lobby group said.
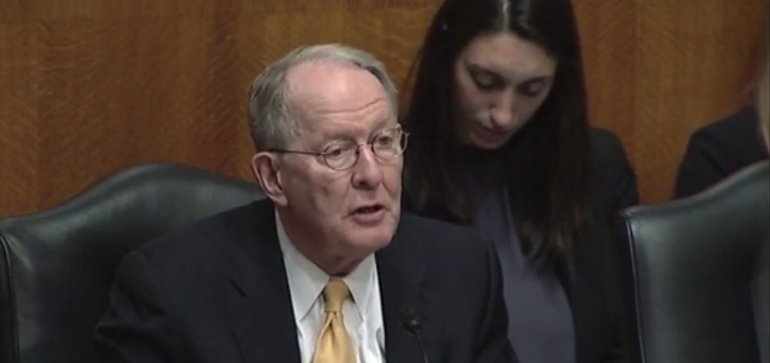
Although the proposed bills have the backing of both parties, a divided Congress and divisive climate in Washington mean an uphill climb for almost any legislation. Still, Senate HELP Committee Chairman Lamar Alexander, R-Tenn., said he hopes to move the package through the committee next month and get it to the Senate floor in June.
“These are common sense steps we can take, and every single one of them has the objective of reducing the health care costs that you pay for out of your own pocket,” he said.
Regardless, the suggested policies can further the debate on hot topics like price transparency and surprise billing.
The senators’ surprise billing law — like other recent drafts — would ban the practice and hold patients harmless, but punts on some of the thorniest issues like arbitration and payment rates.
It includes three options the committee is considering for payment resolution: an in-network guarantee, independent dispute resolution and a benchmark payment.
The in-network guarantee would require hospitals ensure that every practitioner in the facility is considered in-network. The benchmark payment option sets rates based on the median contracted fee for services in the geographic area.
Health policy experts applauded the creation of a national all-payer claims database. The provision is a big deal, Zack Cooper, health economist and associate professor at Yale, said on Twitter . “Hard to land a plane without instruments. Hard to steer a health system without data,” he said. “This is crucial for reducing health care costs.”
AMGA, which represents physician practices, also wrote in support of legislation that would mandate the database, saying it would give “members a tool they have been asking for to help provide the best possible care to the communities they serve.”
The draft bill taking on drug pricing bans pharmacy benefit managers from using spread pricing — charging health plans or patients a different price from what the PBM paid for the drug. It also requires 100% pass-through of rebates to plan sponsors. The lobby group for PBMs said Thursday it is still reviewing the legislation but generally believes “employer clients in the private sector should have choices in designing health benefits” and supports greater transparency throughout the drug supply chain.
The Jefferies analysts said those provisions could be a drag on PBM margins over a transition period.
