The immune system normally defends the body against everything from microscopic viruses to meters-long parasitic worms. But sometimes, it sets its sights on the wrong target: the body’s own cells.
Autoimmunity problems cause many different diseases, depending on which cells are targeted. In Type 1 diabetes, it’s beta cells. Beta cells are located in the pancreas and produce insulin, the molecule necessary to convert food into energy. Without it, patients must monitor their blood and inject themselves with insulin multiple times a day.
Scientists at the Harvard Stem Cell Institute (HSCI) want to develop a better treatment: transplanting healthy beta cells grown in the laboratory into patients. Having figured out the first part of the process, they are now figuring out how to protect newly transplanted cells from autoimmune attack.
Autoimmune epidemic
Arlene Sharpe is the George Fabyan Professor of Comparative Pathology at Harvard Medical School. She said that over the past 30 years, autoimmune diseases have become almost epidemic.
“They’re increasing in frequency and occurring earlier in life, and we don’t understand why,” she said. “There’s tremendous need to understand the causes of these diseases and how to treat them.”
Sharpe said that in the case of Type 1 diabetes, using a patient’s own stem cells — which have the ability to become many types of cells — is a promising therapy. By coaxing the stem cells to become beta cells in the lab, researchers can give patients their own source of insulin.
“One of the challenges now is to be able to deliver these cells in such a way that the body tolerates them,” Sharpe said. “It’s leading to a whole new field of immunology: regenerative immunology.”
Protecting the beta cell
HSCI co-director Douglas Melton, who discovered how to make beta cells from stem cells in 2014, is now turning his attention to the immunity problem. He said that scientists still do not understand exactly how the immune system attacks beta cells.
“We’ve decided to protect the beta cell without knowing all the different ways that the immune system is trying to kill it. We want to genetically modify the beta cell to make it invisible to the immune system,” said Melton, who is the Xander University Professor in the Harvard Department of Stem Cell and Regenerative Biology.
One of Melton’s approaches is to take molecules that are already known to protect cells from the immune system in certain situations, and add them to the beta cells. Pregnancy is a familiar example. A pregnant woman’s immune system does not attack the fetus, even though half of the fetus’s genes come from the father and are foreign to her. The fetus survives because it expresses protective molecules. Cancer cells survive for a similar reason. They express molecules that allow them to evade detection by the immune system.
Searching for new genes
The Melton lab is also searching for entirely new ways of protecting beta cells, using an experiment called a genetic screen.
“When we grow cells to transplant them into a person, we grow a lot of them: around 500 million,” Melton said. “We’ve removed one gene at a time from each cell. Since there are only 20,000 genes, we could do that easily with 500 million cells.”
Most of the mutated cells would be killed by the patient’s immune system.
“But wouldn’t it be fantastic if there was some mutation that said to the immune system, ‘You can’t see me — leave me alone!’” he said.
Testing the genes
Nayara Leite is a postdoctoral researcher in Melton’s lab. She is developing a method to test whether any of those genetic modifications protect beta cells from immune attack.
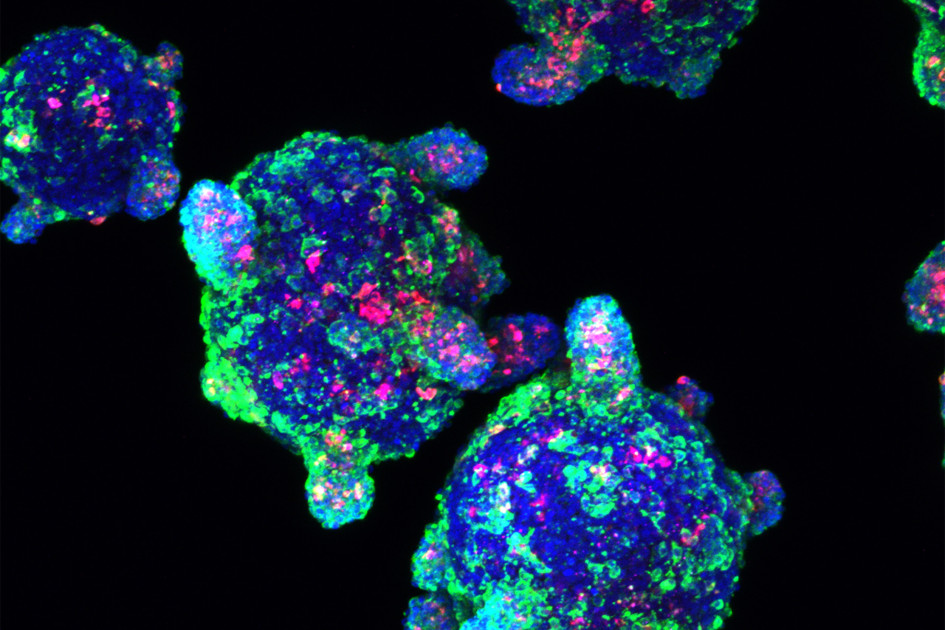
Leite uses blood donated by patients with Type 1 diabetes for two purposes: isolating immune cells, and making stem-cell-derived beta cells.
