U.S. hospitals may not have the capacity to deal with the spread of the novel coronavirus if big changes are not implemented immediately, some of the nation’s leading scientists and policy experts are warning.
Plans are needed urgently across the nation to mitigate the effect the pathogen will have on local health systems. Early research on how the outbreak unfolded and taxed hospitals in China can serve as a guide to better predict and inform response plans here —and the results are alarming.
“If a Wuhan-like outbreak were to take place in a U.S. city, even with strong social distancing and contact tracing protocols as strict as the Wuhan lockdown, hospitalization and ICU needs from COVID-19 patients alone may exceed current capacity,” researchers from Harvard and Johns Hopkins wrote in a paper earlier this month.
The need for care and resources may be higher in some cities, especially those with a higher volume of vulnerable populations — and with populations that are older and with multiple underlying chronic conditions.
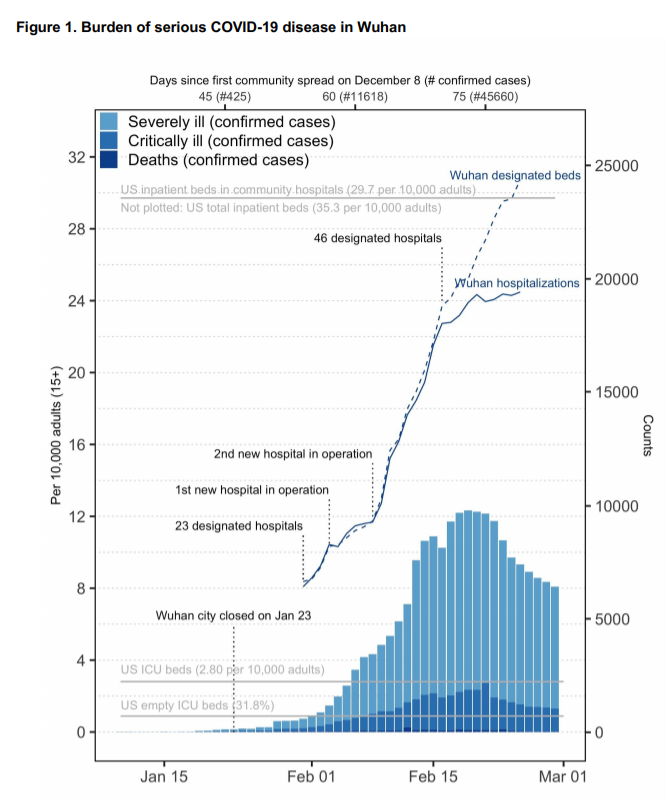
“Even after the lockdown of Wuhan on January 23, the number of seriously ill COVID-19 patients continued to rise, exceeding local hospitalization and ICU capacities for at least a month,” researchers reported.
What makes the modeling so concerning is that Wuhan enacted extreme measures by locking down the city six weeks after “sustained local transmission.” Still, even with that strict measure in place and social distancing mandates, hospitalizations ballooned.
During the outbreak’s peak in Wuhan, nearly 20,000 COVID-19 patients were hospitalized with 10,000 in severe or critical condition, according to the paper authored by Marc Lipsitch, epidemiology professor and director of the Center for Communicable Disease Dynamics at the Harvard T.H. Chan School of Public Health, along with researchers including those from Johns Hopkins Center for Health Security.
The U.S. has a total of 5,198 hospitals, which includes academic medical centers, and about 792,000 beds. That includes 65,000 ICU beds, according to data the American Hospital Association provided Healthcare Dive.
Comparing other nations, the U.S. has about 2.8 hospital beds per 1,000 residents while China has 4.3 per 1,000 residents and Italy has 3.2, according to the Organisation for Economic Co-operation and Development.
Discussions are underway at hospitals systems about how to ramp up capacity, Lyndean Brick, CEO of Advis, a hospital consulting group, told Healthcare Dive.
“We’ve gotten a lot of calls from providers that have shuttered units and may have long-term acute care hospitals that weren’t full, and they’re asking us ‘what are the regulatory steps that we need to take, as well as the operational and security step, to open up these units quickly,'” Brick said.
If President Donald Trump had declared an emergency it would have eased some of the red tape on opening these kinds of units, Brick said.
The biggest worry among hospital leaders is supply chain issues, overcrowded ERs and a shortage of ICU beds, according to an Advis survey.
“What we need now is the federal government to step up in its leadership. And that’s what the survey says,” Brick said.
However, Brian Tanquilut, an analyst with Jefferies, cautioned that hospital capacity in the U.S. for many facilities hovers between 50% to 60% while academic medical centers are typically above 90%.
“As an industry, we have capacity,” Tanquilut told Healthcare Dive, noting occupancy ranges from market to market. “If it really gets acute, I think the issue is not about beds but more about staffing,” he said.
Tanquilut added that some major hospital operators, like HCA and Tenet, have created designated lanes as patients drive up to their facilities. For those who think they have COVID-19, they are swabbed and tested and told to go home to wait for the results as a way not to overtax the hospitals. If their symptoms are severe they are admitted.
Italy’s healthcare system has been pushed to its limits. Physicians have issued recommendations on which patients to prioritize as a shortage of ICU beds and resources persist.
“The criteria include the age of the patient and the probability of survival, and not just ‘first come first served,'” the Associated Press reports on the ethical recommendations published by the Italian society of anesthesiology and intensive care.
In the coming weeks, health officials warned that more Americans will be infected with the disease, exposing hospitals to a potential surge of patients.
“The examples of Wuhan, Italy, South Korea, Japan, and Iran should give us all a strong resolve to slow the epidemic before it is too late,” Lipsitch wrote in an op-ed in the Boston Globe.
Turning point?
Wednesday marked a turning point in the progression of the virus as the World Health Organization characterized it as a pandemic, and cited “alarming levels of inaction” in some countries as cases continue to climb.
On Wednesday, hospital leaders and stakeholders met with White House officials to detail the pain points hospitals may experience over the course of the outbreak in the U.S. and how federal officials can help, according to at least one person in attendance, Byron Jobe, CEO of Vizient, a healthcare company that serves as a consultancy and GPO for health systems across the country.
Leaders discussed a string of issues, including lab testing for COVID-19 and potential problems to the supply chain. They also discussed how to leverage telemedicine as hospitals could become overwhelmed and will need ways to triage and alleviate strain on the system, Jobe told Healthcare Dive.
Many health experts have warned that it’s not too late to try and reduce the spread of the disease.
“If we are complacent and don’t do really aggressive containment and mitigation, the number could go way up and be involved in many, many millions,” Anthony Fauci, director of National Institute of Allergy and Infectious Disease, told a congressional hearing on Wednesday.
The key is now to find the areas with the most coronavirus cases and ramp up response there.
Enbal Shacham, professor of public health and associate director of the Geospatial Institute at St. Louis University, has a paper under review that tries to map potential hot spots for the spread of the coronavirus using predictive modeling with a special focus on vulnerable populations.
The paper outlines that nursing homes closer to an international airport are more likely to have lower quality scores on Nursing Home Compare and therefore may be at a higher risk of disease transmission.
Five nursing home facilities have been struck by the coronavirus in Washington state with 18 deaths at just one facility.
“This is exactly what we were afraid was going to happen,” Shacham told Healthcare Dive.
Many have pointed to a tale of two cities during the influenza pandemic in 1918. The evidence is clear: Philadelphia experienced a significantly higher mortality rate than St. Louis, a city that implemented extreme measures by closing schools, theaters and large public gatherings in the fall of 1918. The difference in response time between the two cities was just 14 days, which made all the difference.
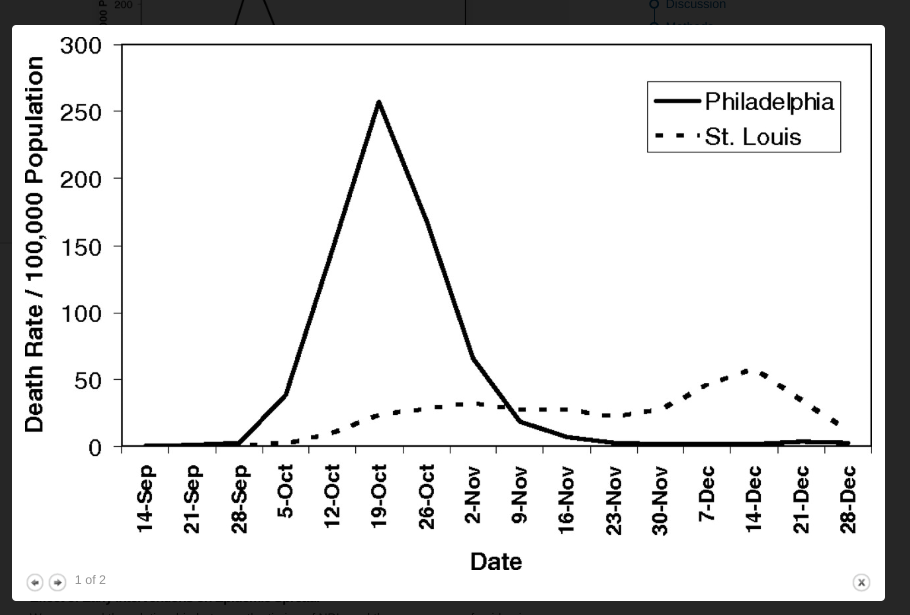
“The costs of this delay appear to have been significant; by the time Philadelphia responded, it faced an epidemic considerably larger than the epidemic St. Louis faced,” according to a previous paper in PNAS.
