Without access to connectivity during the pandemic, too many people could not work for their living, attend school and learn, connect with loved ones, or get health care.
 The COVID-19 era has shined a bright light on what some of us have been saying since the advent of the Internet’s emergence in health care: that digital literacies and connectivity are “super social determinants of health” because they underpin other social determinants of health, discussed in Digital inclusion as a social determinant of health, published in Nature’s npj Digital Medicine.
The COVID-19 era has shined a bright light on what some of us have been saying since the advent of the Internet’s emergence in health care: that digital literacies and connectivity are “super social determinants of health” because they underpin other social determinants of health, discussed in Digital inclusion as a social determinant of health, published in Nature’s npj Digital Medicine.
On the downside, lack of access to digital tools and literacies can increase disparities among people already at-risk for other social determinants of health.
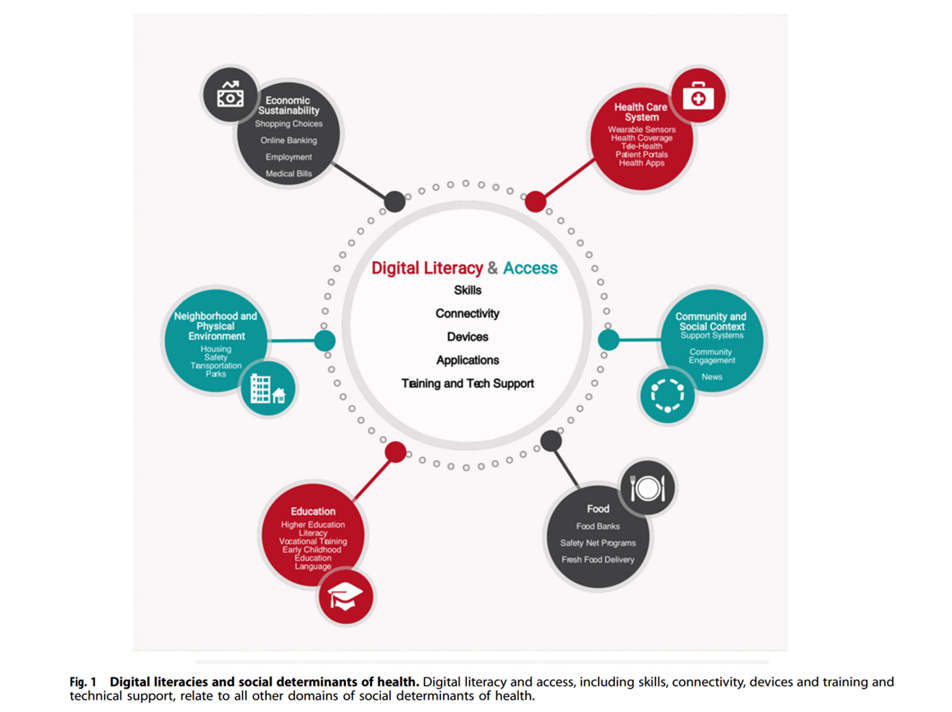
The authors lay out several dimensions of digital literacy and access, including:
- Skills
- Connectivity
- Devices
- Applications
- Training the tech support.
The first illustration, from the paper, illustrates the “super social” impacts that digital literacy and access bolster for SDoH. These bolster,
- Education, from early childhood through vocational training and higher ed
- Neighborhood and physical environment, such as housing and transport
- Economic sustainability, through online banking, employment, and ecommerce shopping options
- Community and social context, enabling engagement and decreasing isolation’s impacts
- Food systems, and finally
- Health care, through telehealth, health education, and wearable sensors that make up the Internet of Things for medical and healthcare.
The team offers policy recommendations, first that healthcare systems adopt digital inclusion and informed strategies to support patients in initial use of digital health tech and sustain that use over time; second, that patients’ levels of health literacy and access to digital literacies be assessed in the clinical context as a medical history question that is embedded in the EHR; and third, that health systems partner with community organizations expert in training digital literacy skills and enabling connectivity. The team points to the National Digital Inclusion Alliance, which maintains a list of organizations providing such training and acts as a clearinghouse for such resources.
Note the timing of this publication: the authors submitted the manuscript to Nature on 19th March 2020….just eight days after the World Health Organization declared the coronavirus a global pandemic.
 Health Populi’s Hot Points: The “super social” adjective was first coined by Dr. Chris Gibbons of Johns Hopkins University, who wrote about Broadband as a Health Imperative back in 2014.
Health Populi’s Hot Points: The “super social” adjective was first coined by Dr. Chris Gibbons of Johns Hopkins University, who wrote about Broadband as a Health Imperative back in 2014.
His vision was spelled out in this illustration, portraying broadband’s potential impact as a “force multiplier” to drive innovation and help the underserved.
This concept informs the current discussion about how we define “infrastructure” moving forward. Fifty+ years ago, we conjured up bridges and roads for cars and trucks, telephone lines and dams.
Enter the digital era, forcing a re-definition of what we mean by “infrastructure.”
It is impossible to disconnect the so-called “care economy” from the larger macroeconomy in the U.S. Health care costs consume nearly one in every five dollars of the American economy. The nation is aging, and disparities and health inequities in the K-recovery are widening.
Consider just one metric on this: the striking differences in the loss of life expectancy for White people compared to Black and Latinx people living in the U.S.
The pandemic worsened the existing gap in life expectancy between Whites and people of color in America, research published by the National Academy of Science has attested.
Investing in broadband upstream becomes that “force multiplier” by enabling people to access information, learn, socially connect (to bolster mental and emotional health), order groceries from a home located in a food desert, and indeed, access medical services and support for well-being and self-care.
At the start of COVID-19 in the U.S., the FCC had identified connectivity gaps in the pandemic as a barrier to both economic and physical health. In building back better, connectivity bolstering care — care of children, care of aging parents, care for our unwell fellow health citizens — is infrastructure meriting investment, with a hard ROI on national and household economies alike.
