A study has concluded that HIV self-testing is safe, increases testing uptake and increases the yield of HIV positive results among men who have sex with men (MSM) and transgender people. Among female sex workers, results are more mixed. While HIV self-testing improves testing uptake, it does not increase the yield of positive results and it worsens linkage to care outcomes.
The study was recently published by Dr Charles Witzel from the London School of Hygiene and Medicine and colleagues in BMC Medicine.
Background
Globally, more than five million people still do not know they have HIV. Key populations remain disproportionately impacted by HIV. In 2018, 54% of all new infections in the world occurred among MSM, people who inject drugs, people in prisons, sex workers, transgender people, and their partners.
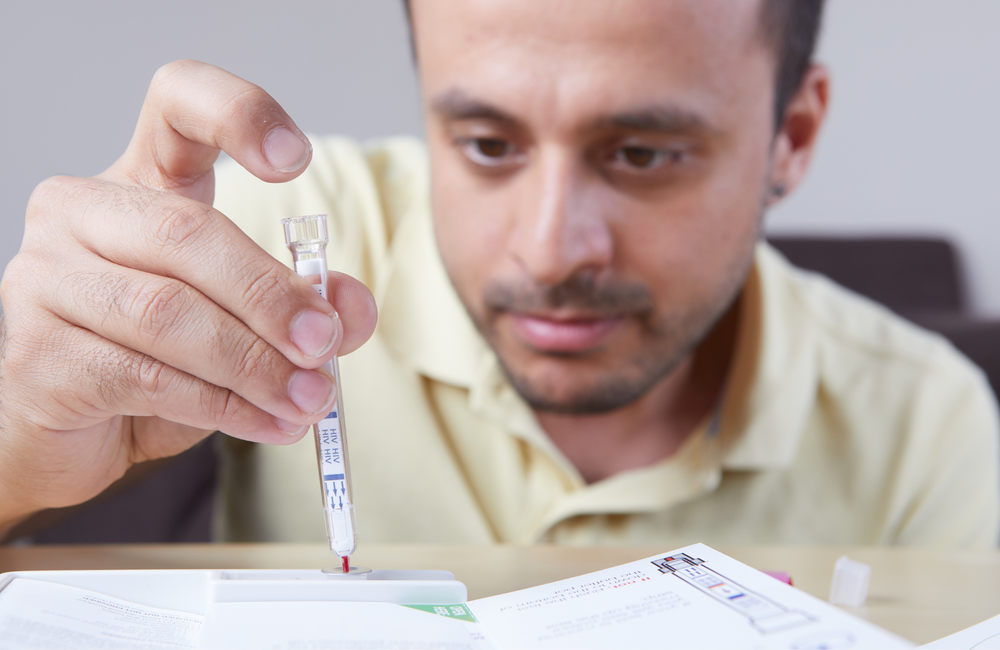
Scaling-up HIV testing among key populations remains urgent. In 2016, the World Health Organization (WHO) added HIV self-testing to its recommended testing approaches. The method is safe, effective, acceptable, convenient and private. It may be particularly attractive to populations experiencing discrimination and stigma, including when seeking HIV testing. However, by mid-2019, only 38 countries had implemented HIV self-testing. Was further evidence needed?
Witzel and colleagues conducted a systematic review of randomised controlled trials that compared HIV self-testing with standard HIV testing in key populations. The objective was to understand the outcomes of HIV self-testing versus standard facility-based HIV testing for key populations. The results informed the WHO 2019 testing recommendations.
The team reviewed trials published in academic journals and conferences up to June 2019. The trials were eligible only if they reported on one or more of the following outcomes: HIV testing uptake, HIV testing frequency, HIV positivity, linkage to treatment or care, STI testing uptake and frequency, condom use, social harm or adverse events.
Results
Ten randomised clinical trials met the eligibility criteria. They had enrolled 9679 participants, of whom 5486 were MSM, 72 transgender people (mostly transwomen) and 4121 female sex workers. No trials with people who inject drugs or people in prisons were found.
To align with the clinical trials, this study reports MSM and transgender people as one group.
There were seven trials with MSM: six in high-income settings and one in China. The three studies with female sex workers were run in Kenya, Uganda and Zambia. All trials used oral fluid-based HIV self-test kits and provided kits free of charge.
In five studies, kits were distributed through healthcare facilities; in five studies (all with MSM) they were ordered online and sent by post; and in two studies (both with female sex workers) they were also distributed by peers. The interventions featured diverse components including promotion on social media, information about HIV testing, group demonstrations of self-testing, videos, pre and post-test counselling and telephone hotlines.
When compared with standard of care, HIV self-testing increased HIV testing uptake by 1.45 times in a meta-analysis of all ten trials (RR=1.45; 95% CI 1.20, 1.75). These results were similar in subgroup analyses of female sex workers and MSM/transgender people. But the largest increase in uptake was found with online/mail HIV self-test distribution among MSM and transgender people (RR=1.61; 95% CI 1.33, 1.94).
For testing frequency, a meta-analysis of three trials – all with MSM – showed that HIV self-testing increased the mean number of HIV tests by 2.56 during follow-up (95% CI 1.24, 3.88). In two trials with facility self-test distribution, this increase was lower (by 2.1 and by 1.7). But the most significant increase, multiplying mean number of tests by 3.80, was found in the one delivering self-test through mail.
“HIV self-testing appears to engage segments of the population with pronounced barriers to standard testing services.”
The meta-analysis of nine trials reporting the proportion of positive results among those tested showed that self-testing had no effect on the yield of positive results. This was different in a subgroup analysis of seven trials run among MSM: the HIV self-testing arms yielded more than double the rate of positivity, compared to standard of care (RR=2.21; 95% CI 1.20, 4.08). In subgroup analyses of trials with MSM, based on online/mail self-test distribution, this rate increased by 2.21 times, as compared to standard of care. The investigators found no significant differences for this positivity rate between peer or facility-based self-testing delivery, compared to standard of care.
There was a meta-analysis of six trials measuring linkage to HIV care or ART among people with a positive result. It found that HIV self-testing reduced linkage to care by 17% (RR=0.83; 95% CI 074, 0.92). Population subgroup analyses showed a 16% (RR=0.84; 95% CI 0.75, 0.94) reduction among female sex workers, and non-significant results for MSM.
The impact of HIV self-testing on STI testing was mixed. Two trials among MSM showed no differences in STI testing between HIV self-testing and standard of care. Another trial run with MSM reported fewer STI tests from the self-testing arm than from the standard of care arm.
There was no impact of HIV self-testing on condom use, either in female sex workers or MSM.
Two trials (both with female sex workers) reported on social harm and adverse events. There were cases of intimate partner violence and mental distress in a few participants using HIV self-testing. Some cases were reported as directly caused by the use of HIV self-tests. But differences between trial arms were not significant.
What next?
“Among key populations, HIV self-testing appears to engage segments of the population with pronounced barriers to standard testing services while increasing choices,” Witzel and colleagues conclude. However, they also highlight that “some significant gaps exist in the evidence which implementation, pilot and demonstration projects can respond to.”
- While transgender people are a population with strong testing needs, the clinical trials recruited very few of them, and did not report their results separately from MSM.
- No trials have been done with people who inject drugs or people in prison – although these two groups may find HIV self-testing acceptable.
- Outcomes of interest in relation to all key populations were not recorded. For example, HIV testing frequency was examined in MSM and a few transgender people, but not in female sex workers.
- The impact of HIV self-testing on STI testing frequency and on linkage to HIV care remains unclear.
In a commentary, Drs Katrina Ortblad and Joanne Stekler from the University of Washington argue that the potential of HIV self-testing is not just to yield positive results and facilitate linkage to treatment. They point out that most people who self-test for HIV will test negative and could benefit from HIV and STI prevention programmes. They may also benefit from mental health support.
“We should also capitalise on the unique characteristics of this testing technology (e.g, privacy, mobility) and utilise HIV self-testing in ways that facilitate linkage to HIV prevention interventions, support health systems, and improve mental health outcomes,” they say.
