Chronic congestive heart failure CHF is a complex disorder characterized by inability of the heart to keep up the demands on it, followed by the progressive pump failure and fluid accumulation. Although the loop diuretics are widely used in heart failure HF patients, both pharmacodynamic and pharmacokinetic alterations are thought to be responsible for diuretic resistance in these patients. Strategies to overcome diuretic resistance include sodium intake restriction, changes in diuretic dose and route of administration and sequential nephron diuretic therapy. In this review, we discuss the definition, prevalence, mechanism of development and management strategies of diuretic resistance in HF patients. The loop diuretics are often used in many patients with chronic congestive heart failure CHF due to their indisputable efficacy in relieving congestive symptoms. In simple terms, diuretic resistance in heart failure HF patients can be explained as a failure of diuretics to control salt and water retention even when used in appropriate doses. It can simply be defined as either a loss of response or reduction in the response to loop diuretics.
J Intern Med ; : — Electrolyte Blood Press ; 13 : 17— Dietary indiscretion and increased oral intake of sodium also can overwhelm the effect of loop diuretics and reduce their their effectiveness. See other articles in PMC that cite the published article. For most diuretics, the secretory pathways have largely been identified and involve organic anion transporters and multidrug resistance proteins. Systems biology of diuretic resistance. He also warned hospitalists to be careful when they see younger heart failure patients those under age 40 or
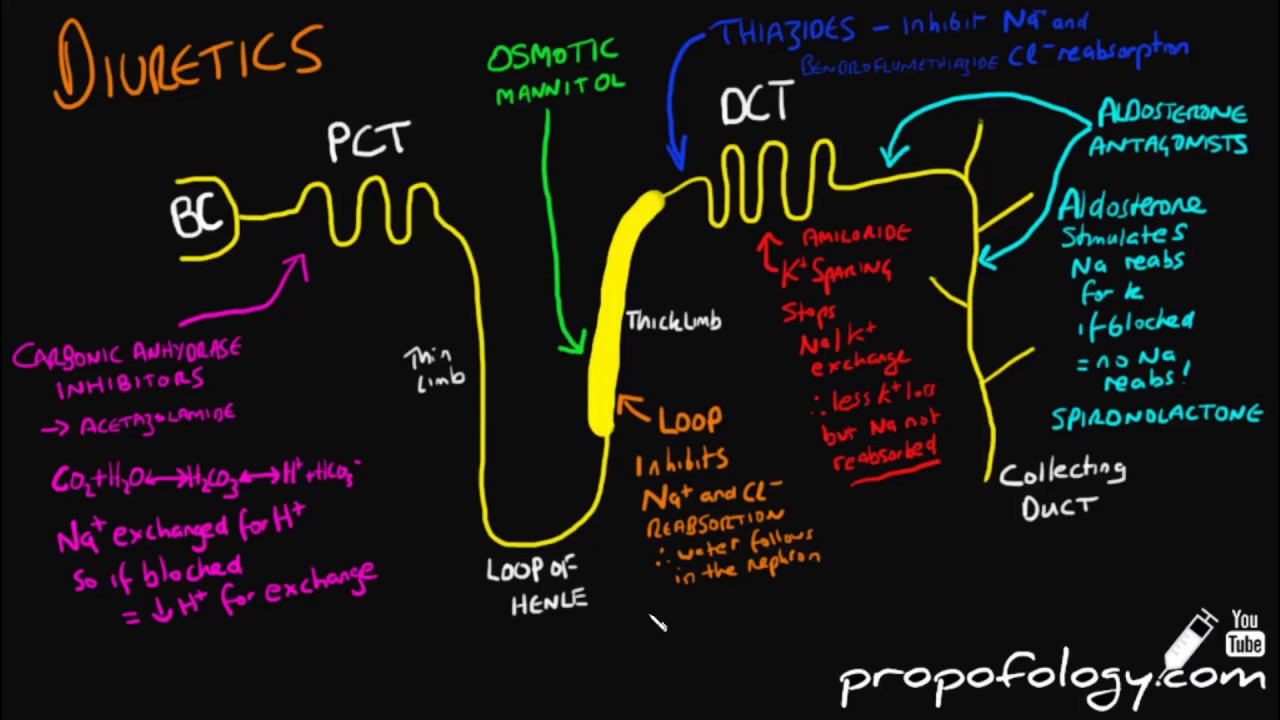
Diuretic resistance is defined as a failure to achieve the therapeutically desired reduction in edema despite a full dose of diuretic. The causes of diuretic resistance include poor adherence to drug therapy or dietary sodium restriction, pharmacokinetic issues, and compensatory increases in sodium reabsorption in nephron sites that are not blocked by the diuretic. To illustrate the pathophysiology and management of diuretic resistance, we describe a patient with nephrotic syndrome. This patient presented with generalized pitting edema and weight gain despite the use of oral loop diuretics. Nephrotic syndrome may cause mucosal edema of the intestine, limiting the absorption of diuretics. He was admitted for intravenous loop diuretic treatment. However, this was ineffective, likely due to compensatory sodium reabsorption by other tubular segments. The combination of loop diuretics with triamterene, a blocker of the epithelial sodium channel, effectively reduced body weight and edema. Recent data suggest that plasmin in nephrotic urine can activate the epithelial sodium channel, potentially contributing to the diuretic resistance in this patient.
